The Medicare 2023 draft physician fee schedule (PFS), proposes changes to policies for telehealth and opioid use disorder treatment. There is also a plan for limited fee-for-service funding that can be used to address social needs.
The draft rule would also expand opioid treatment and recovery services. It would allow for greater use of mobile units such as vans to improve access for those who are homeless or living in rural areas.
CMS stated that the rule proposed by CMS reflects current law. This includes keeping the key conversion factor flat or an update of 0%. The combination of the 3% increase in PFS payments 2022 expiration means that the proposed calendar year 2023 PFS converter factor is $33.08. This represents a decrease by $1.53 from the CY 2022 PFS convert factor of $34.61, CMS stated.
The draft rule will take time for the staff of physician associations to review it fully. However, the American Medical Association (AMA), expressed immediate dissatisfaction with some aspects of the rule.
"It is obvious that the rule not just fails to account for inflation practice costs and COVID related challenges to practice sustainability but also includes a significant, damaging across-the board reduction in payment rates," stated Jack Resneck Jr., MD, President of AMA.
Anders Gilberg is the senior vice president of government affairs for Medical Group Management Association (MGMA). He said that his group is "extremely concerned" about a proposed 4.42% decrease to the conversion factor. This would be during a period of inflation, lingering COVID-19 issues, and a staffing shortage.
Gilberg stated that the proposed cuts and the 4% PAYGO sequestration, which will take effect Jan. 1, 2023, would have a negative impact on group practices.
The draft rule was praised by the National Association of Accountable Care Organizations, (NAACO), in contrast. Clif Gaus (Chairman of the NAACO), ScD stated that proposed changes would allow CMS to achieve its goal of having all Medicare beneficiaries enrolled in a relationship with a clinician responsible for quality and total costs of care by 2030.
CMS estimates that today's changes will save Medicare over $15 billion and generate $650 million in shared savings payments to ACOs. Gaus stated that ACOs are the best alternative payment model because providers are held accountable for patient outcomes throughout the year.
Here's a summary of some of the key policy changes made in the rule proposal:
CMS proposed that several services temporarily made available via telehealth services in the event of a public health emergency (PHE), be made available to users on a Category III basis.
CMS stated that this will give CMS more time to collect data that can support their inclusion as permanent additions on the Medicare telehealth service list. CMS also proposes to extend the time services can be temporarily added to the telehealth services listing during the PHE. However, they will not be included on a Category II, II or III basis for a period 151 days after the end of the PHE.
Proposed rule includes plans to allow licensed professional counselors, mari and family therapists, as well as other types of behavioral healthcare practitioners, to provide behavioral services under general supervision (rather than direct). CMS proposes to pay for licensed clinical social workers and clinical psychologists to deliver integrated behavioral health services as part a patient's primary healthcare team.
CMS stated that it proposes to bundle certain chronic pain management services and treatment services into monthly payments. This will improve patient access to team-based comprehensive chronic care treatment.
CMS stated that the new Healthcare Common Procedure Coding System codes, and the valuation for chronic pain management and treatment services, would encourage more practitioners to accept more Medicare patients with chronic pain. CMS stated that these proposed changes could also encourage Medicare patients with chronic pain to seek out treatment in a partnership to help them manage their condition.
CMS proposes a way for funds from certain Medicare Shared Savings Program ACOs to be used to address social need.
CMS stated in a factsheet that the proposal would provide an opportunity for rural providers to form ACOs and build the infrastructure necessary to support the program. It also promotes equity by holistically meeting patient needs.
CMS proposes that ACOs with smaller populations have greater time to adjust to downside risk. This will help to increase participation in rural and underserved communities. To reward outstanding care provided to underserved communities, the agency proposed an ACO's health equity adjustment to its quality performance category score.
CMS proposes that a follow up colonoscopy to an at home test be considered preventive, meaning that Medicare beneficiaries would not have to pay for it. In line with the new age recommendation of 50, Medicare proposes to cover the service for people 45 and older.
Medicare Part B pays for dental services if they are part of a medically necessary service such as a reconstruction of the jaw after an accident injury.
CMS proposes to include more dental services in the draft 2023 pay rule. This includes examination and treatment prior to an organ transplant.
CMS also wants to hear from the public about other medical conditions that Medicare should cover for dental care, such as joint replacement surgery or cancer treatment. Additionally, CMS will be seeking input on a process to solicit public input on additional dental services that may be necessary for the clinical success and sustainability of other medical services.
CMS stated that it wants to increase total payments for medication-assisted and other opioid use disorder treatments (OUD) as well as recognize the need for longer therapy sessions.
CMS suggested that the rate for individual therapy be adjusted to reflect the severity of OUD in patients who are receiving treatment. The current rate was based on a crosswalk code which describes a 45-minute session.
CMS proposes to allow opioid treatment program (OTP), intake code, to be furnished via audio-video communications technology. This will allow for billing for buprenorphine treatment. This would be applicable if the Drug Enforcement Administration and Substance Abuse Mental Health Services Administration (SAMHSA), authorize the use of audio-video telecommunications to initiate buprenorphine treatment.
In cases where audio-video technology cannot be used, the federal agency proposes to allow the use of audio-only communications technology to initiate buprenorphine treatment.
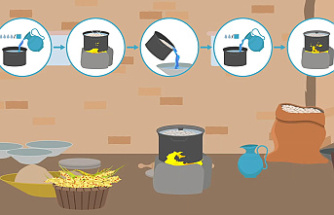
CMS also stated that it would clarify its policy so that opioid treatment programs could bill Medicare for medically necessary and reasonable services furnished via mobile units, in accordance to SAMHSA and DEA guidance. CMS proposes that locality adjustments would apply to services furnished by mobile units, as if they were provided at the physical location where the OTP is registered with DEA and certified SAMHSA.
Kerry Dooley Young, a freelance journalist, is based in Miami Beach. She is the Association of Health Care Journalists' core topic leader for patient safety. Follow her Twitter @kdooleyyoung
Follow Medscape on Facebook, Twitter and Instagram for more information.